In this challenging landscape, community health centers (CHCs) have emerged as beacons of hope, providing accessible and comprehensive healthcare to underserved populations. CHCs have been focused on a more expansive definition of primary care since their inception, weaving behavioral and oral health access into its definition of primary care. They stand at the forefront embracing a transformative approach to care through the adoption of integrated care. These models prioritize whole-person health, seamlessly weaving behavioral health into primary care services.
Integrated care (you’ll also see it described as “holistic care” or “whole-person care”), is a collaborative, top of license medical and business model characterized by extensive coordination, communication, navigation, coaching, intervention and treatment among health professionals, those they treat, and even informal members of the patients care team, like family members. The primary goal is to provide comprehensive discovery, prevention, guidance and treatment that addresses the biological, psychological, and social needs of patients. Health care is too siloed, rarely planned, designed or executed with the “consumer in mind”, which must change. Even CHC’s who have delivered primary, behavioral and dental care for years have to be careful not to confuse co-location of services with integrated care – they are not the same.
According to the American Psychological Association, the “quadruple aim” of integrated care focuses on improving patient access, quality of care, and cost-effectiveness. I argue it’s a higher standard – what economists call “perfect agency” – “what would our patient do if they were imbued with our knowledge.” This describes a higher order relationship expectation – too many providers are transaction-oriented, but integrated care requires a life-cycle mindset.
Here are just three reasons community health leaders continue to integrate new models into practice which prioritize whole-person, collaborative care.
1. Improved Results
The integration of behavioral health into primary care yields benefits for both patients and clinics. By addressing physical and mental health needs together, integrated care models ensure a holistic approach to patient wellness. Mental health issues such as anxiety and depression often coexist with physical conditions, influencing the overall well-being of patients. Recognizing and treating these comorbidities in tandem results in more comprehensive care and improved patient outcomes.
Integrated care also enhances patient engagement and adherence to treatment plans. As mental health services are delivered within the familiar setting of a primary care clinic, patients are more likely to seek help and follow through with recommended treatment. The stigma often associated with visiting a separate mental health facility is reduced, encouraging patients to prioritize their psychological well-being.
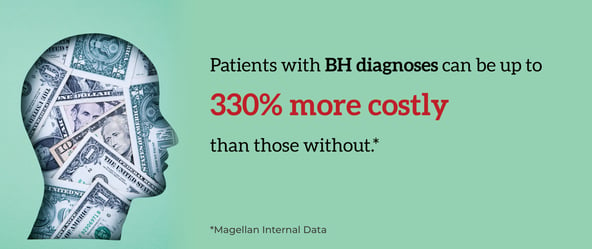
“Too many Americans live in behavioral health deserts – they have little or no access to care. Or, at best, they have access to a fragmented healthcare system, leaving key needs unmet,” said Caroline Carney, M.D., Chief Medical Officer for Magellan Health. “We must address the behavioral, physical and pharmacy needs of people through an integrated approach that augments the important work of providers and supports the member through their entire health journey.”
Integrated care management models, such as Collaborative Care Management (CoCM), promote early detection and intervention. By having behavioral health experts collaborate with primary care providers, potential mental health issues can be identified earlier, preventing them from escalating into severe conditions. This proactive approach not only improves patient outcomes but also reduces the burden on emergency departments and hospital admissions.
2. It’s Not Just a Medical Model, but a Viable Business Model
The financial viability of CHCs is a critical factor in sustaining their mission of serving vulnerable communities. One of the most significant benefits of integrated care models is the creation of more opportunities for revenue. It is imperative that all CHC leaders are focused on growing their businesses in an additive, accretive way; remember, “no margin, no mission”. A clear comparative advantage and natural endowment of CHCs is their role in the primary care hierarchy in their communities – in every community that enjoys a CHC, they boast a significant portion of the collective primary care and prevention capacity – this is one of the reasons why an integrated care business model makes so much sense.
Integrated care models place a strong emphasis on engagement, screening, early detection and intervention of mental health and substance use issues. By making a practice of routinely screening all patients, CHCs can identify latent, undiagnosed mental health conditions. These screenings and assessments, along with any care coordination support provided, can be billed accordingly, creating an additional revenue stream for the clinic (payable by Medicare and a handful of State Medicaid programs).
Further, programs such as CoCM align with the principles of value-based care contracting where patient outcomes and quality of care are rewarded. By adopting CoCM and demonstrating improved patient outcomes, CHCs can negotiate more favorable value-based care contracts, leading to enhanced revenue potential.
3. It’s a Workforce Multiplier
The collaborative nature of integrated care models requires a team-based approach to patient care, allowing CHCs to maximize the potential of their existing workforce, and even the support of community-based stakeholders. CoCM, for instance, involves primary care providers, behavioral health specialists, care coordinators, and other support staff working together cohesively.
When planned appropriately, CHCs can leverage this team-based approach as a workforce multiplier by efficiently utilizing the skills and expertise of each team member, including partners, some of whom may not be employees. This is a classic example of “top of license” care, aligning the appropriate inputs to generate the best output, but also an example of crowdsourcing all available resources – in this case the CHC with its choreographer hat on can summon, command and organize resources from partners and community organizations. Primary care providers can focus on medical issues while behavioral health specialists address mental health concerns, with care coordinators ensuring seamless access, communication and continuity of care. By sharing the workload and responsibilities, the overall efficiency of the health center is significantly improved.
The seamless integration of whole-person, behavioral health into a broader primary care agenda, through innovative models like Collaborative Care Management presents a new opportunity for CHCs. By adopting an integrated care model, health centers can improve patient outcomes, enhance their financial sustainability through increased billing opportunities, and create a dynamic workforce multiplier.
As healthcare systems continue to evolve, CHCs at the forefront of integrated care models are poised to set new standards of comprehensive and patient-centered care. By recognizing the advantages of integration and embracing innovative programs like CoCM, CHCs can better fulfill their mission of providing equitable and accessible healthcare to underserved communities, while securing their own long-term success and sustainability.


.png)


.png)